Anaphylaxis and Food Allergies
In Australia, food allergies affect approximately 1 in 10 infants and 1 in 100 adults.
While some allergies may only cause minor effects like a rash or itching, others can cause a severe and life-threatening condition known as anaphylaxis. The prevalence of food allergies is increasing in Australia at an alarming rate, a phenomenon that researchers are desperately trying to understand.
In the meantime, it is important for people to familiarise themselves with the risks of allergic reactions and how to manage them.
The foods that trigger 90% of food allergic reactions in Australians include:
While peanut, tree nut, fish, shellfish and sesame allergies are usually lifelong, children often outgrow milk and egg allergies.
It is vital that people living with the risk of anaphylaxis, as well as their carers, know how to avoid anaphylactic triggers, how to identify anaphylactic symptoms, and how to respond if an anaphylactic reaction occurs.

If you have anaphylaxis and come into contact with a food that you are allergic to, you may experience the following symptoms:

When it comes to life-threatening food allergies, all stages of food preparation are important. People with anaphylaxis can be so sensitive to certain substances that even slight traces can cause a severe allergic reaction. If you have experienced an anaphylactic reaction from a particular type of food or you have a family history of severe food allergies, you should see a doctor. Your doctor will organise for you to get tests so that you know which foods to cut out of your diet completely.
If you have been prescribed with an auto-injector, you should carry it with you at all times so that when you experience the early signs of anaphylaxis you can administer this shot immediately.
People with anaphylaxis rely on food labels and food outlet staff to provide accurate information about food preparation and content. This information determines whether food is safe for them to eat, however in many cases it is not 100% guaranteed. When it comes to food allergies, the risk can never be completely eliminated. It is therefore important to have your adrenaline auto-injector with you at all times and know what to do in the case of an emergency.
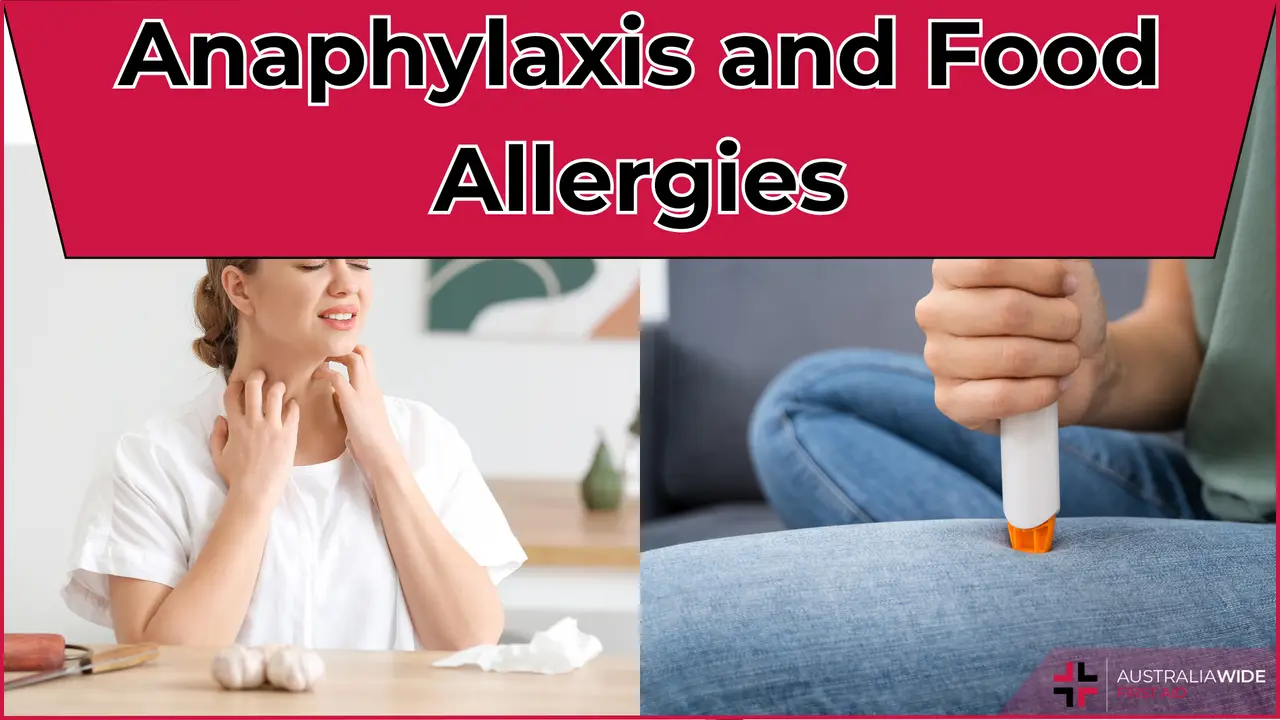
If someone’s symptoms and signs suggest anaphylaxis, you should follow their Anaphylaxis Action Plan or take the following steps:
For more information about managing anaphylaxis read Guideline 9.2.7 by the Australian Resuscitation Council.
If you want a more in-depth look at anaphylaxis at home or in the workplace, our online courses are the answer. You can complete them at your work desk or from the comfort of your own home, and get a Certificate of Completion to show your employer, add to your resume, or simply give you the peace of mind knowing you can actually help in an emergency. Our Anaphylaxis First Aid provides learners with the knowledge needed to recognise, respond to, and manage allergic reactions and anaphylaxis.
If you're after workplace-specific information, our Workplace Anaphylaxis Risk Management course covers responsibilities and best practices for managing anaphylaxis risk in workplaces. Alternatively, our Workplace Asthma and Anaphylaxis Management and First Aid course teaches the essential knowledge and practical tools to identify, manage, and respond to asthma and anaphylaxis risks in workplace settings.
If you're interested in learning more about allergy and anaphylaxis, you might like to check out the following articles in our Resource Library:
Do you want to learn first aid, including how to manage allergy symptoms? Head to one of our regular training courses:
October 2, 2013
In an asthma or anaphylaxis emergency you should know the symptoms, remove triggers, and know how to respond. Read on to understand these important aspects in the context of such an emergency.
May 7, 2024
Asthma, a chronic respiratory condition affecting millions worldwide, is often shrouded in myths and misconceptions. Despite how common it is, there is a distinct lack of common knowledge. This is leading to potential mismanagement and unnecessary anxiety for those living with asthma.

February 19, 2024
For many Australians, our city and outdoor lifestyles come with a hidden challenge – dust allergies. Dust mites, pollen, and other airborne particles can trigger allergic reactions, affecting a significant portion of the population.